Clinical Cut-Offs & Results Interpretation Guide
Evidence-based reference thresholds to support GP decision-making
What Our Physiology Services Mean for Patients
Med-Ex provides objective physiological testing across cardiovascular, respiratory, metabolic and frailty domains.
Each test includes:
-
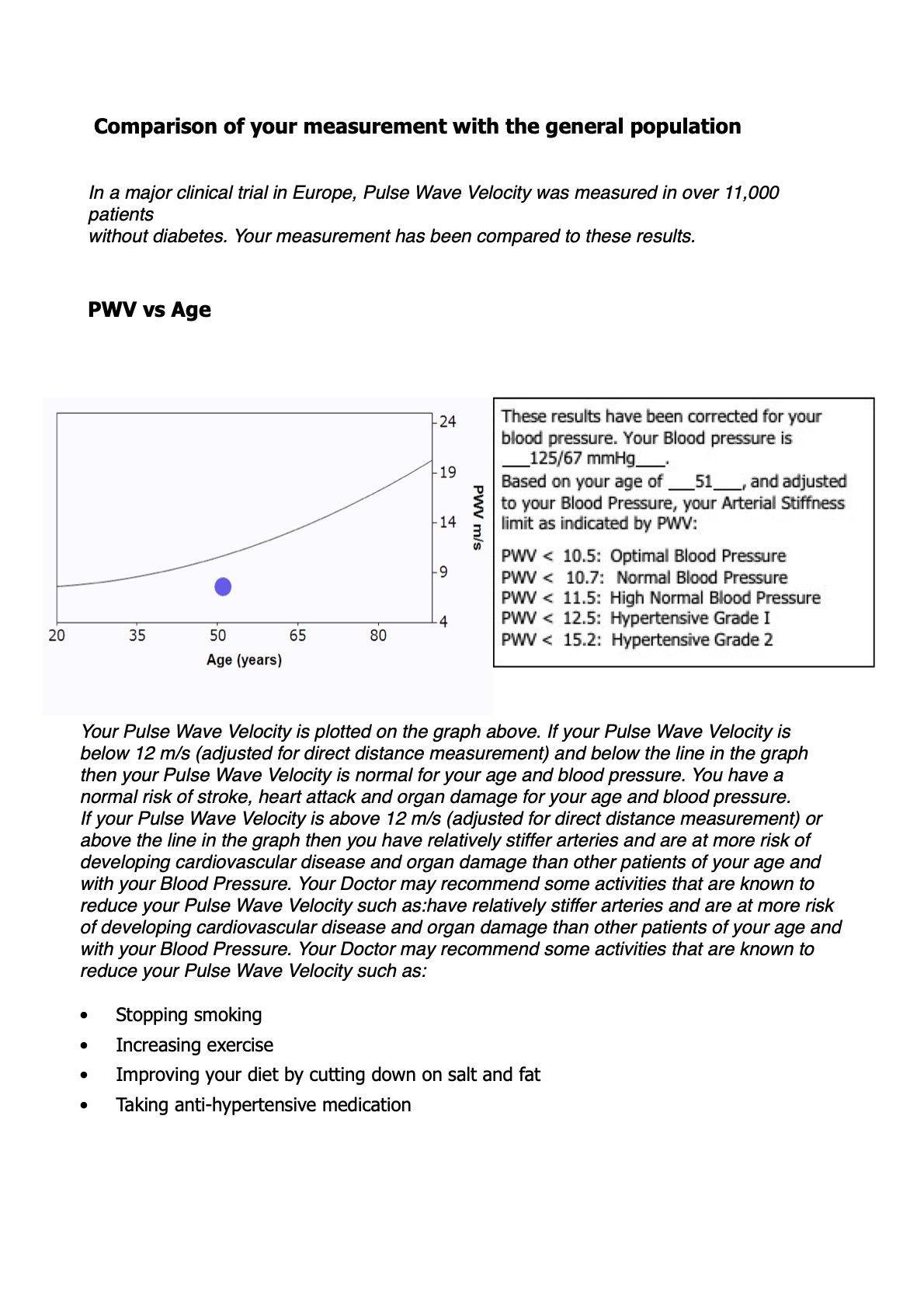
Pulse Wave Velocity (PWV)
Variables: cfPWV (m/s), central BP
Cut-offs (ESC / AHA):
<10 m/s – normal arterial compliance
10–12 m/s – borderline stiffness
>12 m/s – elevated stiffness (CKD, LVH, vascular ageing)
>14 m/s – high-risk phenotype
Why clinically useful:
Predicts CV mortality better than brachial BP
Identifies vascular ageing and CKD progression risk
Important pre-operative risk marker
References: ESC Arterial Stiffness Consensus; AHA Vascular Function Statement.
________________________________
Augmentation Index (AIx / AIx@75)
Variables: Wave reflection magnitude, vascular compliance
Cut-offs:
Men: <25% normal
Women: <35% normal
>40–45% – increased vascular load
>50% – impaired buffering capacity
Why clinically useful:
Predicts peri-operative BP instability
Indicates endothelial dysfunction
Sensitive to autonomic imbalance
References: AtCor Medical; London Arterial Studies.
-
Variables: VO₂peak, Anaerobic Threshold (AT), VE/VCO₂ slope, HRR
Cut-offs (ATS/ACSM):
VO₂peak (% predicted)
80% normal
60–80% mild impairment
40–60% moderate
<40% severe (major surgical risk)
Anaerobic Threshold (AT)
11 mL/kg/min → low risk
8–11 → moderate risk
<8 → high peri-operative risk
VE/VCO₂ slope
<30 normal
30–36 moderate inefficiency
36 prognostic marker (HF, PH, CKD)
Why clinically useful:
Best predictor of peri-operative mortality
Essential for risk stratification before TEER, major orthopaedics, and cancer surgery
Quantifies metabolic and ventilatory reserve
References: ATS/ACCP CPET Guidelines; ACSM; HF Consensus.
-
Variables: FEV₁, FVC, FEV₁/FVC ratio
Cut-offs (ATS/ERS):
FEV₁ % predicted:
80% normal
70–79 mild
60–69 moderate
50–59 moderately severe
<50% severe
FEV₁/FVC <0.70 → obstructive defect
Why clinically useful:
Identifies airflow obstruction
Provides objective baseline for anaesthesia and surgery
Vital for TEER and major ortho pre-assessment
References: ATS/ERS Spirometry Standards.
-
Variables: 24-hour BP, dipping index, AASI, morning surge
AHA ABPM cut-offs:
24h avg <130/80
Day <135/85
Night <120/70
Dipping:
Normal: 10–20%
Non-dipper: <10%
Reverse dipper: ↑ BP at night (major risk)
Morning Surge:
55 mmHg = stroke risk
AASI:
<0.40 normal
0.40–0.50 borderline
0.50 arterial stiffness
Why clinically useful:
Detects masked hypertension
Predicts renal decline
Strong predictor of stroke and MI
References: AHA 24-hour BP Guidelines; Kario MSURGE.
-
(Use age 70–85 normative tables)
Chair Stand (30s)
≥10 normal
8–9 mild frailty
≤7 frailty
8-Foot Up-and-Go
≤6 sec normal
7–9 mild
≥10 frailty
≥12 high fall risk
2-Minute Step Test
≥60 steps normal
40–59 moderate
≤39 frailty
Why clinically useful:
Predicts surgical outcomes
Predicts readmission risk
Identifies mobility decline
References: Rikli & Jones Senior Fitness Test Manual.
-
Variables: static/dynamic balance, postural control
4-Stage Balance Test (CDC/WHO)
Fail tandem ≥10 sec → impairment
Single-leg <5 sec → fall risk
Single-leg <2 sec → severe frailty
Why clinically useful:
Predicts fall risk > 2 years
Indicates vestibular/autonomic dysfunction
References: CDC STEADI; WHO Falls Guidelines.
-
Gait Speed (4 m)
0.8 m/s normal
0.6–0.8 pre-frail
<0.6 frail
<0.4 severe frailty
TUG
<10 sec normal
20 frail
30 very high fall risk
Why clinically useful:
Best single predictor of loss of independence
Strong predictor of mortality in frail older adults
References: Fried Frailty Criteria; Podsiadlo & Richardson (1991).
-
HRV
RMSSD <20 ms → parasympathetic withdrawal
SDNN <30 ms → low autonomic resilience
LF/HF >2.5 → sympathetic dominance
Orthostatic
SBP drop ≥20 mmHg OR DBP ≥10 mmHg → OH
HRV recovery >2 min → autonomic blunting
Why clinically useful:
Predicts falls, syncope, peri-op instability
Tracks autonomic neuropathy & recovery
References: Task Force on HRV (1996); autonomic dysfunction literature.
Example; part of a test result for Joe Blogs
Gold Standard BP and Vascular Testing
Combing arterial stiffness and BP to determine systemic load
Let’s Work Together
If you're interested in working with us, complete the form with a few details about your patient. We'll review your message and get back to you within 48 hours.